Amazing Mammal Mothers Making Milk
By Rosalie Rust You may have heard someone say that breastfeeding our babies is a basic human right. However, it isn’t uniquely human. In fact,… Read More »Amazing Mammal Mothers Making Milk
By Rosalie Rust You may have heard someone say that breastfeeding our babies is a basic human right. However, it isn’t uniquely human. In fact,… Read More »Amazing Mammal Mothers Making Milk
By Sharon Knorr, IBCLC One of the things that we can depend on, unfortunately, is that disasters and emergencies will continue to happen around the… Read More »Disaster Preparedness: Breastfeeding Matters During an Emergency
By Norma Ritter IBCLC, RLC This article is part of a series on Weaning and Starting Solids:1 of 3: When is the Best Time to… Read More »Thinking About Weaning?
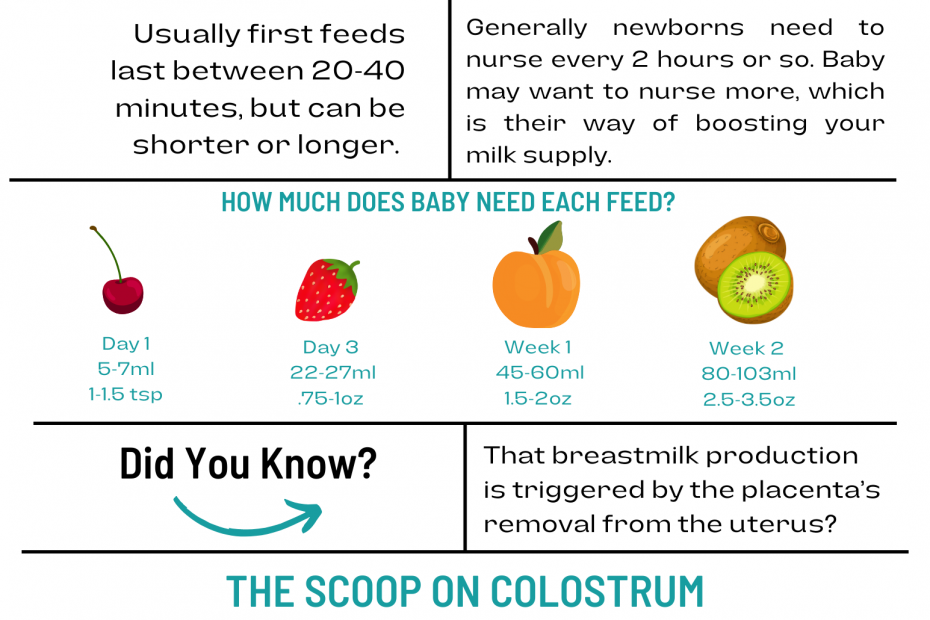
Breastfeeding in the early days can be a challenge! Check out this cheat sheet for information on beginning.

Three steps to paced bottle feeding!

So, you need some pumping hacks? We’ve got you covered!
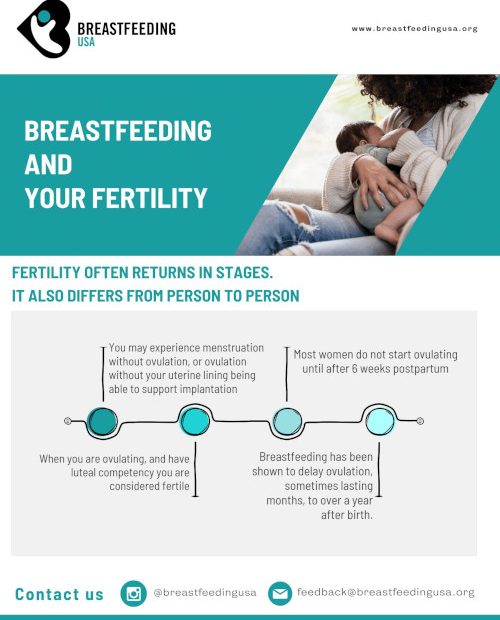
Fertility often returns in stages. It also differs from person to person.

Can you breastfeed after drinking? Do you need to pump and dump? The answers are a bit complicated. Here’s what we know.
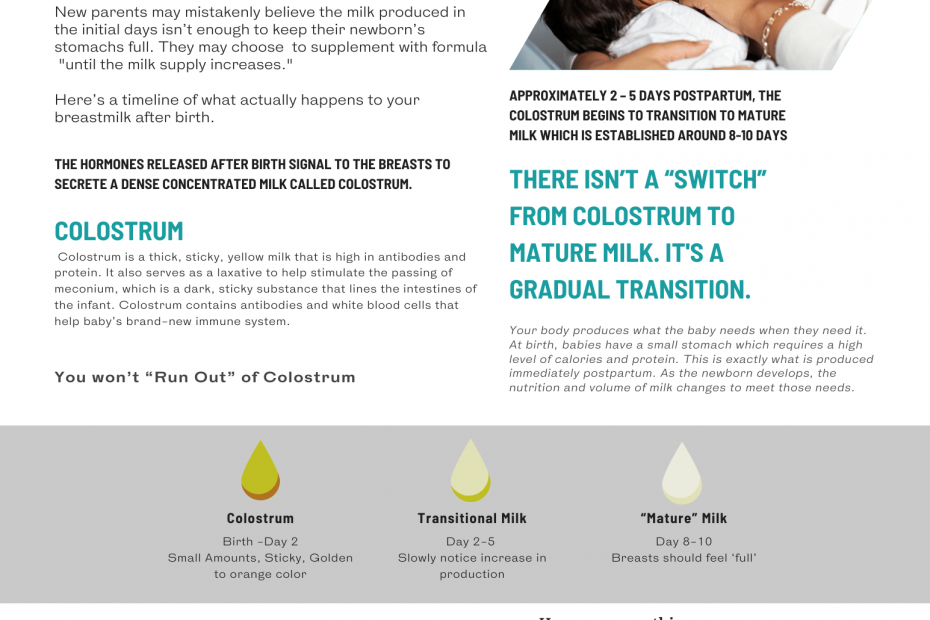
What to expect in the first few days of breastfeeding.